In 2017, an estimated 10 million people contracted tuberculosis with 1.6 million eventually dying from the condition. This makes tuberculosis the world’s deadliest infectious disease and one of the ten leading global causes of death. Of this number, more than 95 per cent of cases and deaths are recorded in countries of the Global South.
For this reason, the UN’s Sustainable Development Goals (SDGs) have prioritised combating tuberculosis and other diseases. By 2030, the SDGs hope the fight against the epidemics of AIDS, tuberculosis, malaria and other communicable diseases will be successful; with the sub-goal of Objective 3 of the SDGs aiming to ensure a healthy life for all people of all ages and to promote their well-being.
Tuberculosis is transmitted through the air by a bacterium that in most cases affects the lungs. It is therefore enough for a person suffering from pulmonary tuberculosis to cough or sneeze in order to infect other people in the immediate vicinity. This is what makes the disease so dangerous – it can spread very quickly. People with a weak immune system are, in particular, susceptible to the disease, for example people living with HIV, malnutrition or diabetes. But the disease can be treated and prevented. The World Health Organization estimates that between the years 2000 and 2017 about 54 million lives could have been saved through the diagnosis and treatment of tuberculosis.
One issue, especially in countries of the Global South, is that treatment takes a long time. In order to prevent a relapse and the patient developing a resistance to the bacteria, different antibiotics have to be taken for up to six months. In countries with poor healthcare systems, however, there is often a lack of trained personnel to accompany patients and monitor regular use of the drugs. In recent years, this has led to an increase in multi-resistant pathogens against which antibiotics have no effect. Multi-resistant tuberculosis can also be treated, but in these cases more comprehensive treatment is necessary.
NimCure – a Digital Care Tool
Nigeria is one of the 30 countries with the highest incidence rates of tuberculosis. According to the WHO, about 418,000 people in the country in sub-Saharan Africa have contracted the disease. The Nigerian Institute of Medical Research (NIMR) has now joined forces with the Co-Creation Hub (CcHUB), an innovation centre in Lagos. The aim of this partnership is to develop and manage a digital tool to support and improve compliance of tuberculosis patients with treatment in Nigeria.
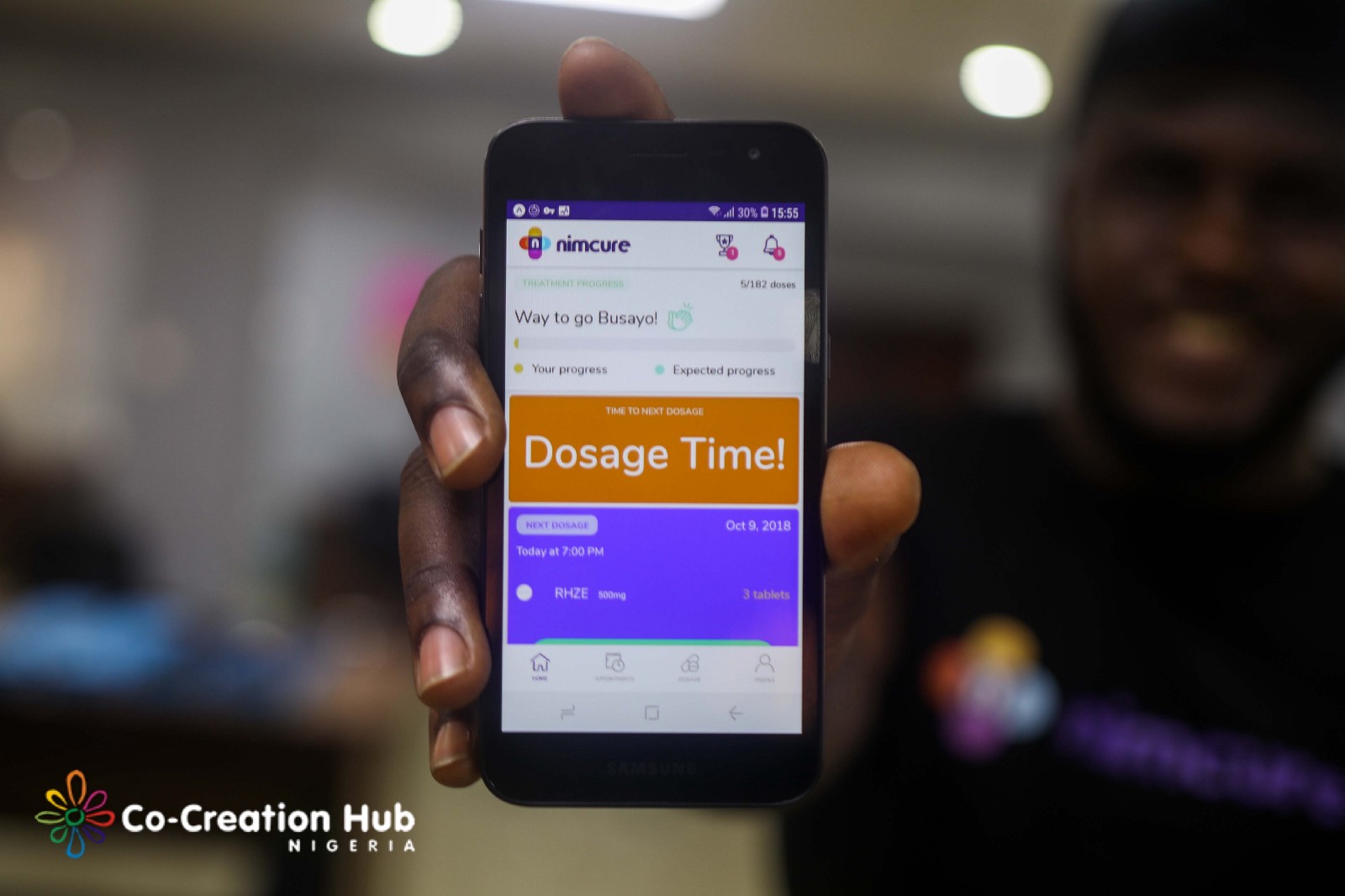
The resulting NimCure app was launched this month in conjunction with a medical study involving 30 patients and six caregivers. The app connects patients with caregivers who support and manage their treatment remotely. Patients can also record short videos to record their daily dosing. In addition, the app allows patients to track treatment progress, receive important notifications and reminders, and contact their nurses. Nurses themselves can use the app to monitor patient treatment, evaluate video submissions, manage patient treatment progress, and contact patients directly. This will enable more people to receive medical care or monitoring, especially in rural areas where the medical infrastructure is not well developed. For the duration of the pilot project, patients and caregivers will be equipped with mobile phones and internet data.
Since smartphones and the internet are becoming increasingly important – especially in Africa – the app could actually save many lives. It remains to be seen how the pilot phase will proceed, which is scheduled to last eight months, and how the app will be used later. Not all people in Nigeria can afford a mobile phone and expensive data packages, even if the number of phone users in the country continues to rise.
This article is a translation by Mark Newton of the original article by Jasmina Schmidt which first appeared on RESET’s German language site.